1
Washington Apple
Health Guide to
Unwinding from the
PHE
What happens to Apple Health
(Medicaid) eligibility starting in 2023
as Washington State Moves ForWArd
Version 3: Released 05/18/2023

2
Updated versions can be found at: hca.wa.gov/phe
For questions, comments, or concerns on the information in this guide, email
AHEligCovi[email protected]ov
.
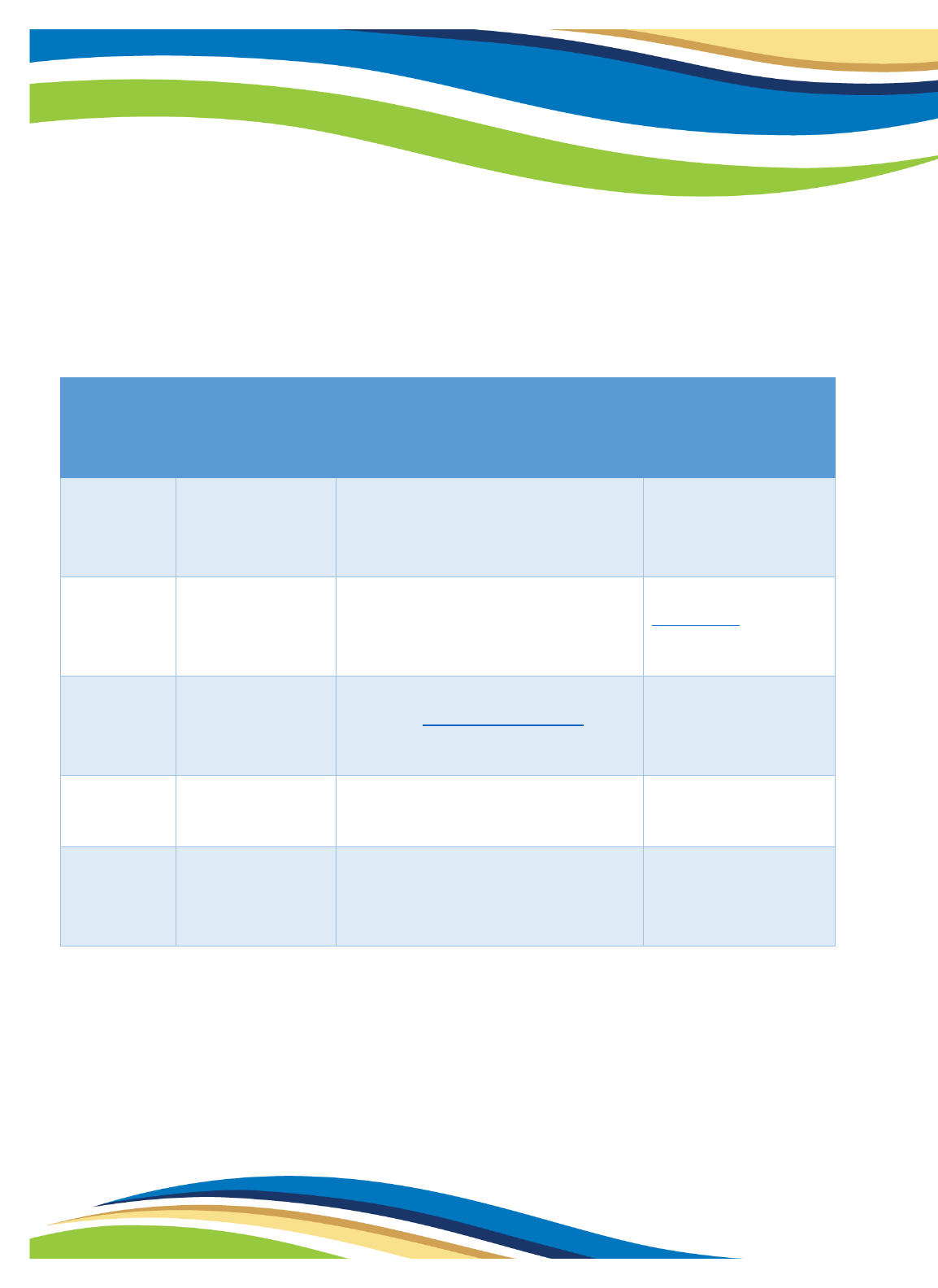
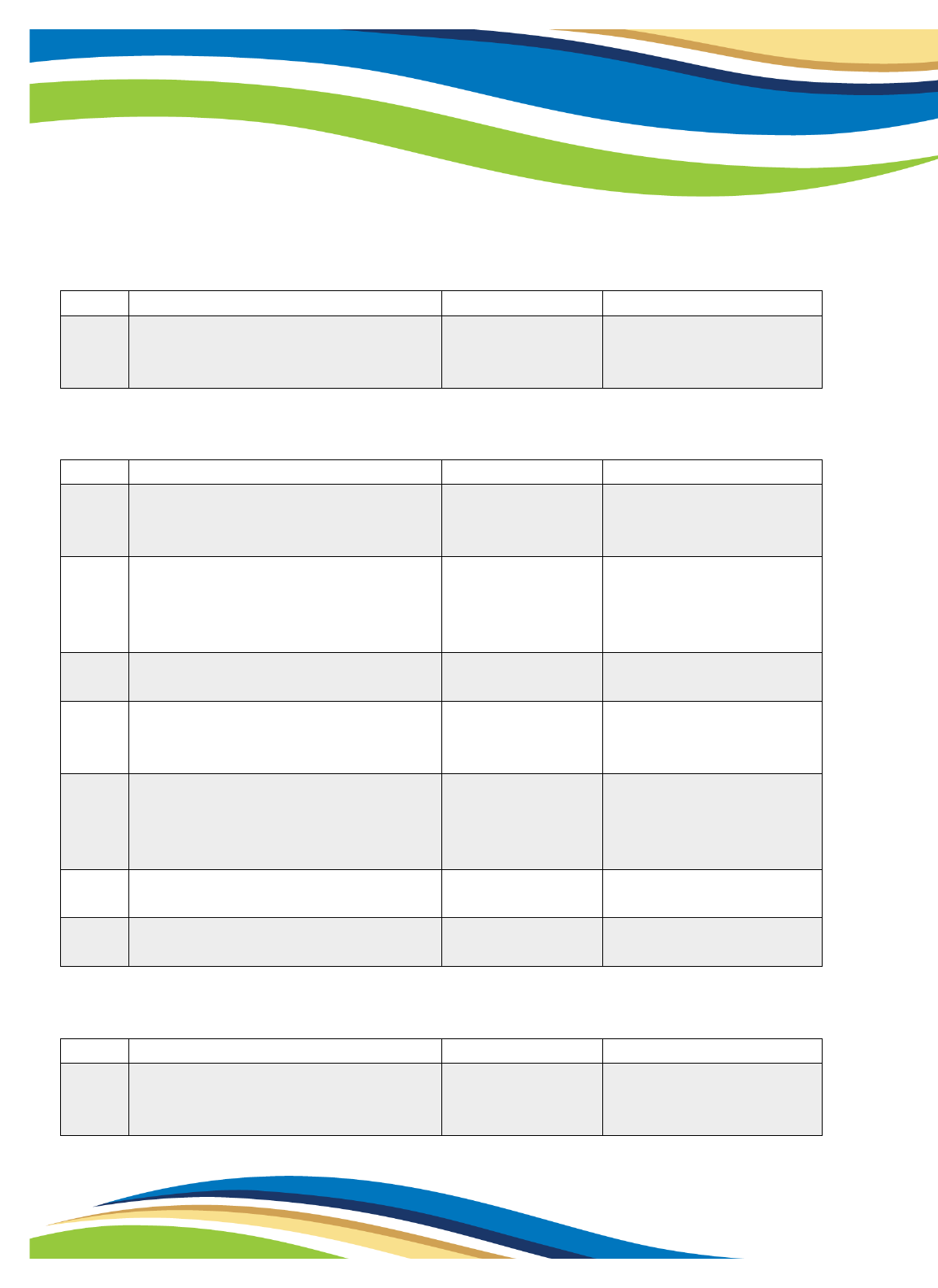
Change log
Version
Page No.
What Changed
Reason for Change
3
10
Added in language about Classic Apple
Health renewal
Incorporated ex parte renewal
overview
3
11, 16
Updated dates for renewal outreach
Process finalized after last published
version of guide
3
14, 20, 26
Updated references to Covid-19 testing
and treatment
Covid-19 testing and treatment
coverage under AEM ends with the
public health emergency
3
18
Deleted dates for domestic production
activities deduction
Activity was completed.
3
25
Updated dates relating to premiums
Policy and procedures finalized after
last published version of guide
3
26
Added section on returned renewal
mail
Policy and procedures finalized after
last published version of guide
3
27
Updated section with webinar info
Webinars already occurred
Important note!
This document is updated as much as possible. For any issues, email
In March 2020, the Families First Coronavirus Response Act allowed Medicaid to continue
if the public health emergency (PHE) continued. Federal rules separated the continuous
Medicaid requirement from the PHE and required states to begin redetermining
eligibility as of April 2023.
3
3
28
Outreach (texts, MCO) timeline updated
Processes finalized after last published
version of guide
3
36
Updated image of envelope
Version 3 has updated image of
envelope
3
40, 42
Updated description for Apple Health
letters
Clarified difference between Apple
Health requests for information letters
3
Appendix 3
Updated with current version of
eligibility reviews
Text change slightly for eligibility
reviews since last publication
3
Throughout
Corrected hyperlinks
3
Throughout
Updated with date PHE ended
HHS ended the PHE after the last
published version of the guide
3
Appendices
4, 7
Added images of postcards
Developed after last published version
of guide
3
Throughout
Corrected hyperlinks
3
Throughout
Updated with date PHE ended
HHS ended the PHE after the last
published version of the guide

4
Contents
How to use this guide ..................................................................................................................... 7
Overview ......................................................................................................................................... 8
PHE background and Apple Health impact .................................................................................... 8
New changes .................................................................................................................................. 8
Unwinding ...................................................................................................................................... 8
Chapter 1: Classic Apple Health coverage through DSHS ............................................................... 9
Eligibility Reviews (ER) .................................................................................................................... 9
Outreach ....................................................................................................................................... 11
Resuming normal operating procedures – Classic Apple Health ................................................. 12
Clients receiving Long-term services and supports (LTSS) ........................................................... 14
General reminders ....................................................................................................................... 14
Alien Emergency Medical (AEM) – Classic ................................................................................... 14
Chapter 2: MAGI Apple Health through Washington Healthplanfinder....................................... 15
Renewals ...................................................................................................................................... 15
Resuming normal operating procedures – MAGI ........................................................................ 18
Post-eligibility reviews (PER) ........................................................................................................ 19
ProviderOne extensions ............................................................................................................... 19
After-Pregnancy Coverage (APC) ................................................................................................. 20
Alien Emergency Medical (AEM) – MAGI ..................................................................................... 20
Foster care (FC) and adoption support (AS) ................................................................................. 20
Moving to a Qualified Health Plan ............................................................................................... 21
Chapter 3: Moving between Classic and MAGI Apple Health programs ...................................... 23
Apple Health for Adults (N05) and 65+ or Medicare-eligible ...................................................... 23
SSI terminations ........................................................................................................................... 23
MAGI Apple Health and LTSS ....................................................................................................... 24

5
Chapter 4: Other Classic and MAGI Apple Health program information ..................................... 25
Language access ........................................................................................................................... 25
CHIP and HWD premiums ............................................................................................................ 25
Public charge ................................................................................................................................ 26
Appeals ......................................................................................................................................... 26
Reconsideration ........................................................................................................................... 26
Returned renewal mail ................................................................................................................. 26
Upcoming webinars ...................................................................................................................... 27
Contact .......................................................................................................................................... 27
Outreach ....................................................................................................................................... 28
Apple Health ambassador program ............................................................................................. 29
MCOs and 834 information .......................................................................................................... 29
Appendices .................................................................................................................................... 30
Appendix 1: Coverage groups ...................................................................................................... 30
Appendix 2: MAGI renewal notices, PER notice, and outreach ................................................... 36
New enhanced envelope .......................................................................................................... 36
Washington Apple Health Renewal – Review Only (EE008)..................................................... 37
Response Required: Apple Health Renewal (EE009) ................................................................ 38
Washington Apple Health Termination (EE011) ...................................................................... 39
Post-Eligibility Review – Response Required: Apple Health Request for Information (EE005) 40
Response Required: Apple Health Request for Information (EE005) ...................................... 42
Appendix 3: Classic Eligibility Review notices and outreach ........................................................ 43
Mail-in Eligibility Review (0022-01) .......................................................................................... 43
Mail-in Eligibility Review (0022-04) .......................................................................................... 44
Appendix 4: Notices to CHIP and HWD clients ............................................................................. 45
Healthcare for Workers with Disabilities (HWD) premium postcard ....................................... 45
Apple Health for Kids with Premiums (CHIP) postcard ............................................................ 46

6
Appendix 5: Redetermination Notice to ProviderOne extensions .............................................. 47
ProviderOne redetermination notice ....................................................................................... 47
Appendix 6: Notice to MAGI Apple Health for Adults who are 65+ or Medicare eligible ........... 48
Medicare FAQ notice ................................................................................................................ 48
Appendix 7: Postcard sent prior to renewal/eligibility review .................................................... 50
End of PHE Postcard (MAGI) ..................................................................................................... 50
End of PHE Postcard (Classic) ................................................................................................... 51
Appendix 8: Acronyms ................................................................................................................. 52
7
How to use this guide
This guide is for external use by navigators, brokers, providers, managed care organizations
(MCOs), tribal entities, and other stakeholders. It is maintained by staff within Health Care
Authority’s (HCA) Office of Medicaid Eligibility Policy (OMEP). This guide is all inclusive and may
contain information not applicable to you or your organization.
The guide is divided into four different sections:
1. Apple Health Classic Medicaid (non-Modified Adjusted Gross Income (MAGI)) clients
who apply with the Department of Social and Health Services (DSHS), including
through Washington Connection.
a. Including clients who receive long-term services and supports (LTSS) through
Home and Community Services (HCS) or Developmental Disabilities
Administration (DDA) and all other Classic Apple Health Programs through
DSHS’ Community Services Division (CSD).
2. MAGI clients who apply for coverage through Washington Healthplanfinder.
3. Clients who need to move between MAGI and Classic Apple Health (Medicaid).
4. Miscellaneous information that applies to both Classic and MAGI Apple Health clients.
A list of common acronymns are in appendix 8.
We are readily available to assist with any training, review, or meetings to clarify any information
in this guide. Email AHEligCov[email protected] to arrange a time for review or address any
questions, comments, or concerns.
Note: Nothing in this guide is intended to provide legal rights to any person or entity. The guide is
intended solely for informational purposes and should not be relied upon as the basis for any
legal action. Eligibility policies and procedures are governed by federal and state statutes,
regulations, and formal sub regulatory guidance.

8
Overview
PHE background and Apple Health impact
The Department of Health and Human Services (HHS), a federal agency, determined COVID-19 to
be a public health emergency (PHE) starting in January 2020. The PHE ended May 11, 2023.
The Families First Coronavirus Response Act (FFCRA) allowed most Apple Health clients to
continue receiving Apple Health coverage for the duration of the PHE. This is called “continuous
enrollment.” Certain eligibility and verification factors were also relaxed. Apple Health no longer
terminated clients who failed to renew or complete an eligibility review. If a client’s eligibility
terminated for any other reason, HCA and DSHS reopened coverage, unless the client passed
away or moved out of state.
New changes
In December 2022, Congress signed into law the Consolidated Appropriation Act, 2023, which
separates the continuous enrollment requirement from the PHE. This required Washington state
to begin redeterminations 04/01/2023.
Unwinding
HCA worked closely with the Washington Health Benefit Exchange (HBE), which operates
Washington Healthplanfinder, and DSHS to develop post-PHE plans to redetermine clients’
eligibility for Apple Health. We are calling this “unwinding” from all the changes that occurred
during the PHE.
HCA will utilize new and improved ways of reaching clients, including automated phone calls, text
messages, enhanced envelopes, and updated correspondence. The goal is to ensure clients
respond to renewals and eligibility reviews to see if they are eligible for continued Apple Health
coverage or other insurance through Washington Healthplanfinder.
9
Chapter 1: Classic Apple Health coverage
through DSHS
Who
Clients eligible for Classic (non-MAGI) Apple Health coverage are those who are:
• Age 65 or older; or
• Have blindness or a disability and are not eligible for MAGI coverage through
Washington Healthplanfinder; or
• Eligible for Medicare.
Classic Apple Health coverage includes clients receiving long-term services and supports (LTSS),
which is administered by Home and Community Services (HCS) and Developmental Disabilities
Administration (DDA). DSHS’ Community Services Division (CSD) administers all other Classic
Apple Health programs. DSHS also administers some programs to children who have disabilities
and/or need long-term services and supports.
See appendix 1 for a list of medical programs administered by CSD, DDA, and HCS.
Eligibility Reviews (ER)
During the PHE
ER processes continued, but clients were not terminated for failing to provide an ER.
Unwinding
HCA and DSHS will take up to 12 months to redetermine eligibility for clients who were reinstated
during the PHE. This process is based on clients’ post-PHE review end dates. Clients go through
the ER process based on their system-assigned review end date.
ER processes began in April when DSHS mailed ER notices to clients due for review 05/31/2023.
The ER notice is updated to include language about the PHE ending; see appendix 3 for a copy of
10
the notice. This includes eligible clients, clients active on coverage only because of the PHE, and
those receiving state-funded LTSS.
DSHS staff will first attempt to renew eligibility for clients without the client needing to provide
an ER form. This is called an ex parte or administrative renewal. Staff will look to see if data
matches show a client can be renewed on the same coverage group(s). If the data matches show
a client cannot be renewed or would change to a coverage group with lesser services, the client
will need to submit an ER.
DSHS sends ERs by mail 45 days before a client’s certification end date. Copies of ER notices are
also mailed to authorized representatives when one is on file. The system mails a termination
notice at least 10 days before the end of the month to anyone who has not submitted their ER.
Terminations for not submitting an ER resume 05/31/2023 for clients due to renew by
05/31/2023. Assigned HCS and DDA staff follow equal access policy and contact clients if their
annual eligibility review is not received.
Key takeaways
• May, June, and July will have a higher than usual number of ERs mailed and
received compared to August-onward.
• Terminations for not renewing eligibility resume 05/31/2023 for clients due to
renew 05/31/2023.
• Clients reinstated solely due to the PHE will have eligibility redetermined at their
next ER.
11
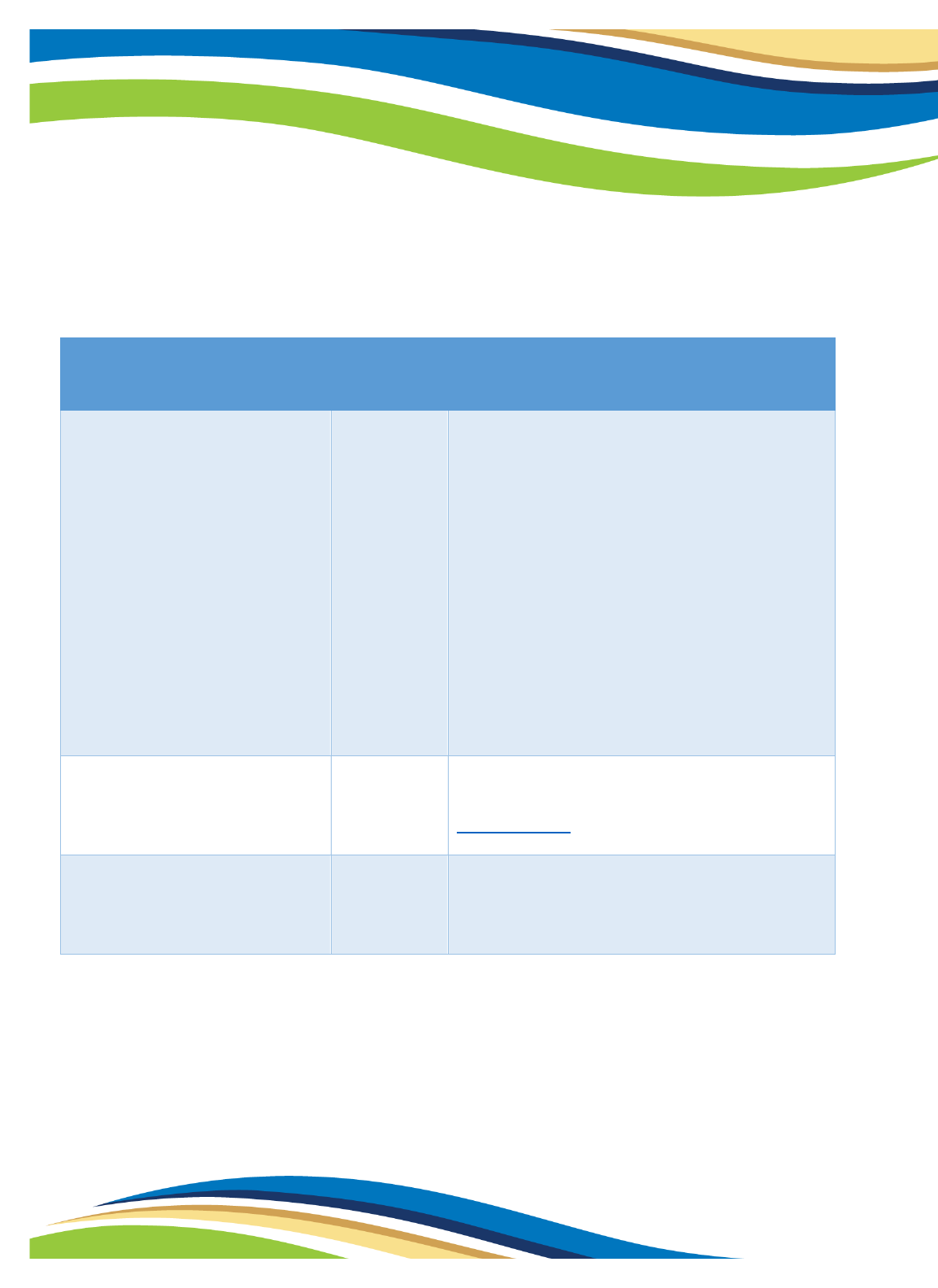
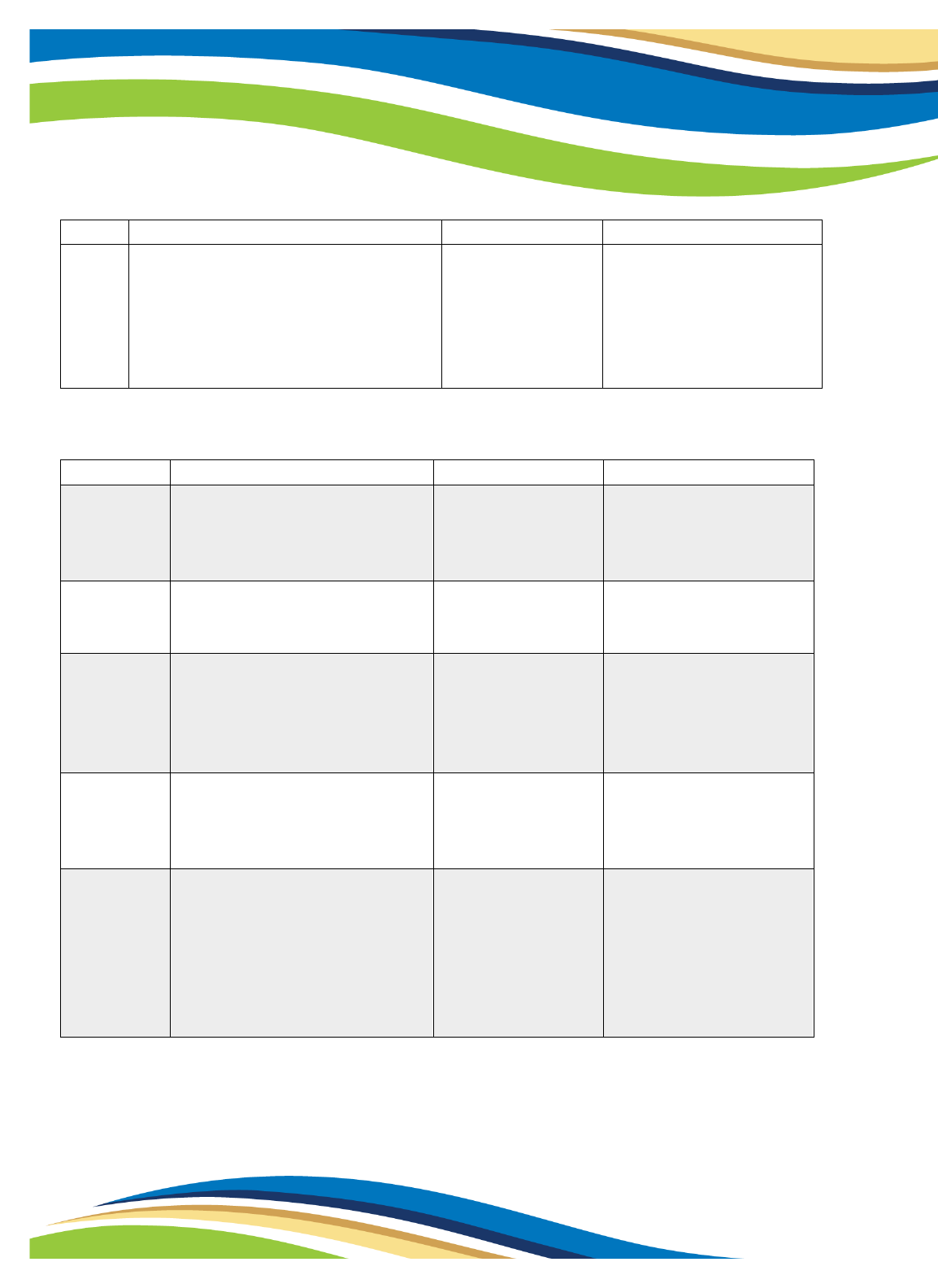
Outreach
DSHS and HCA will complete the below activities for the 12 months beginning with clients due for
review 05/31/2023. The goal is to encourage responses to ER notices.
Days before
certification
end date
Example of ER
due by
05/31/2023
Activity
Outreach method
85
03/06/2023
Contact information update
campaign: are your address(es) and
phone number(s) up to date
Postcard via USPS
49
04/12/2023
Mail-in ER notice goes out with new
added text about need to respond
Letter via USPS; see
appendix 3 for an
example
20
05/09/2023 to
05/11/2023
Text message reminder to complete
ER. Go to hca.wa.gov/ah-texts for
more information.
Text message from
HCA
16
05/15/2023
Reminder calls begin to complete ER
DSHS – CSD
automated call-out*
10
05/21/2023
Termination letter for not renewing
goes out to those who did not
submit an ER
Letter via USPS
*DSHS – CSD begins automated call campaign to clients who have not had their ER initiated. The prerecorded
message will remind the client to submit their ER and how to do it as well as providing an option to connect to an
agent to complete their renewal over the phone.
Note: This automated call will not be initiated to HCS and DDA clients. Assigned Public Benefits
Specialists for HCS follow equal access policy and contact clients if their annual eligibility review is
not received.
12
The above activities are in addition to any statewide outreach to clients by managed care plans
and HCA, such as social media posts encouraging clients to respond to any notices.
Resuming normal operating procedures – Classic Apple Health
During the PHE
Staff accepted self-attestation of income, resources, and medical expenses.
Key takeaways
• Staff began requesting verification of income, resources, and other eligibility factors
on 04/01/2023, unless they can be verified through electronic data sources.
• Change reporting requirements and case action on reported changes resumes.
• Some terminations resumed 04/30/2023, but more likely 05/31/2023.
13
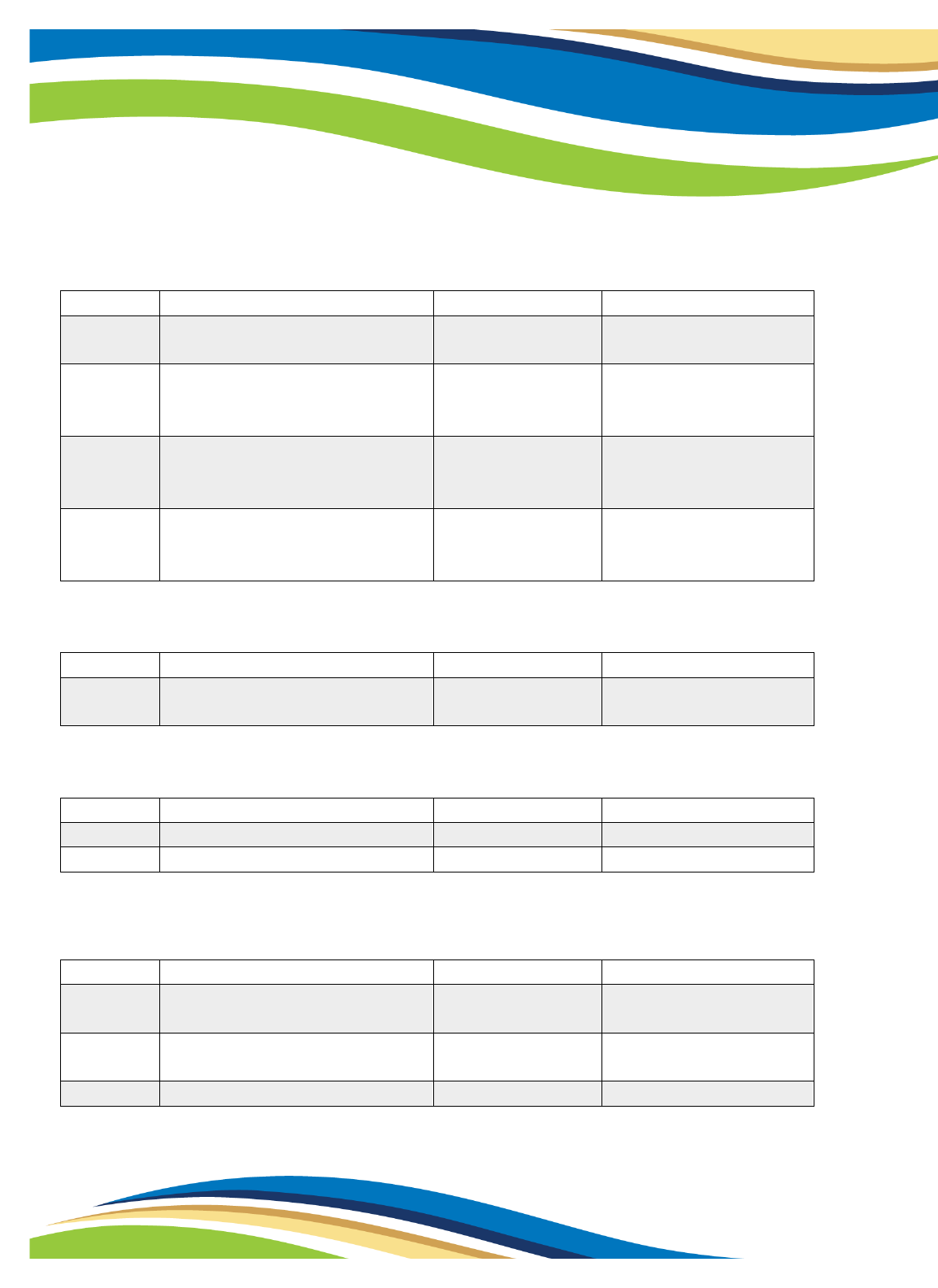
Unwinding
Beginning 04/01/2023, staff resumed requesting verification of income, resources, medical
expenses, and other eligibility factors, unless staff can verify through electronic data sources.
Procedure
Resume
date
Details
Verification of medical
expenses, income, and
resources
04/01/2023
DSHS began requesting verification of medical
expenses, income, and resources if the
information cannot be verified through
electronic data matches. If a client reports
their employer or source of income is
unavailable (i.e., business closed), DSHS will
take self-attestation as allowed prior to the
PHE. DSHS will provide clients with more time
if requested to provide verification and can
take self-attestation, if needed. Staff may also
accept self-attestation and allow 30 days to
provide needed verification.
Return mail
04/01/2023
Terminations for whereabouts unknown
resume effective no sooner than this date. See
Returned Mail.
Change reporting requirements
and case action on reported
changes
04/01/2023
If a client has not had a medical ER completed
in the last 12 months and a change is reported
that impacts eligibility, an ER may be initiated.
14
Clients receiving Long-term services and supports (LTSS)
• When return mail is received, staff use two methods to verify the client’s whereabouts.
They first try to call the client and authorized representative, and if unable to reach
anyone, they will contact the assigned social service case manager for updated client
contact information. If contact is unsuccessful, clients may be terminated.
• As of 4/1/23, staff began requesting verification, including proof of earned income, court
orders for guardianship fees, and certain resources if information cannot be verified
through electronic data sources.
• Staff will accept self-attestation of most unearned income types, liquid resources and
primary residence, and some expenses, if the information can be verified through
electronic data sources.
• Assigned HCS and DDA staff follow equal access policy and contact clients if their annual
eligibility review is not received.
General reminders
• Clients terminated for not providing verification have until the date of termination to
provide the verification. They can also request an extension. If information is provided,
DSHS will review to see if the client remains eligible.
• Clients may reapply at any time.
Alien Emergency Medical (AEM) – Classic
AEM clients will receive one final ER notice with text shown in appendix 3; see Eligibility Reviews
(ER) process. AEM coverage ends with 10 days’ notice if clients do not respond to an ER, request
for medical evidence, or are not clinically eligible.
Note: Coverage under AEM of COVID-19 testing and treatment ended May 11, 2023. Inpatient
hospital services relating to COVID-19 testing and treatment are still covered.
15
Chapter 2: MAGI Apple Health through
Washington Healthplanfinder
Who
Adults under age 65 without Medicare, children, pregnant individuals, or parents and caretakers
get coverage through the Washington Healthplanfinder online application, administered by the
Health Care Authority (HCA). Income eligibility is based on modified adjusted gross income
(MAGI). This includes clients on Washington Apple Health for:
• Family/Caretaker Relatives
• Family/Caretaker Relatives – Extension
• Pregnant Individuals and After-Pregnancy Coverage
• Newborns
• Kids
• Kids with Premiums
• Alien Emergency Medical
• Adults
• Family Planning Only – HCA processes applications, not through Washington
Healthplanfinder.
Renewals
Key takeaways
• May, June, and July will have a higher than usual number of renewals compared to the
August-onward.
• Terminations for not renewing eligibility resume 05/31/2023.
• Clients receiving Apple Health solely due to the PHE may have eligibility redetermined at
their next renewal or change report, whichever occurs first.
16
During the PHE
Renewal processes continued, but clients were not terminated for failing to renew. If they did not
attempt to renew, the system extended Apple Health 3 months at a time.
Unwinding
HCA will take up to 12 months to redetermine eligibility for MAGI clients who were reinstated
during the PHE based on clients’ post-PHE renewal dates. Clients go through the renewal process
based on their system-assigned renewal end date.
The regular renewal processes continue: Between 04/03/2023 and 04/10/2023, Washington
Healthplanfinder attempts to auto-renew clients due for renewal by 05/31/2023. Auto-renewal is
when the system looks at a household’s self-reported income and compares it to available data
sources. If the self-attested income and data sources both show income is under the limit, the
client auto-renews, and the system sends the “Washington Apple Health Renewal – Review Only”
notice.
Procedure
Resume
date
Details
Pre-PHE renewal processes
04/03/2023
Washington Healthplanfinder will attempt to
auto-renew clients due for renewal in May.
Renewal notice
04/10/2023
If a client cannot be auto-renewed,
Washington Healthplanfinder sends the
“Response Required: Apple Health Renewal”
by this date.
Text message reminder
05/09/2023
to
05/11/2023
Text message reminder to complete renewal.
Go to hca.wa.gov/ah-texts for more
information.
Termination letters
05/10/2023
Washington Healthplanfinder sends the
“Washington Apple Health Termination” letter
to clients who did not respond.
Reminder calls begin
05/18/2023
Phone call reminder to complete renewal

17
Terminations for non-renewal
05/31/2023
Clients who did not complete their renewal will
have coverage terminated.
What happens when a client needs to take action to renew?
There are three routes clients take after receiving the “Response Required: Apple Health
Renewal” notice:
1. They can take action to renew and are determined eligible for Apple Health based on self-
attestation.
• If their attestation is not compatible with state or federal sources, they may have
to respond to a post-eligibility review letter. This letter is sent within the following
few weeks and requires a response within 15 days.
2. If they take action to renew and no longer qualify for Apple Health, coverage terminates
at the end of the month.
• Washington Healthplanfinder will offer them additional coverage options, which
may include coverage through a Qualified Health Plan with possible savings
provided under the American Rescue Plan Act (ARPA) and Cascade Care Savings.
• Clients who meet the criteria for Classic Apple Health, such as age or Medicare
eligibility, are given the choice to be referred to DSHS’ Washington Connection.
3. If they do not respond, Apple Health terminates at the end of the month for not
renewing.
What happens after termination for not renewing?
Clients terminated for not renewing have 90 days from the termination date to complete their
renewal and be retroactively reinstated from the termination date, if they are still eligible,
without a gap in coverage.
• For example, a client who terminates 05/31/2023 for not renewing has until 08/31/2023
to complete their renewal. If eligible for Apple Health, they are automatically approved as
of 06/01/2023.
18
Domestic Production Activities (DPA) deduction
HCA added a “domestic production activities” income deduction to some applications to keep
Apple Health active during the PHE. This deduction is no longer allowed and will be automatically
removed from applications. Client eligibility will not be redetermined until the next renewal or
change report.
Resuming normal operating procedures – MAGI
Procedure
Resume
date
Details
HCA began requesting
verification
04/01/2023
Request verification for income, deductions,
and medical expenses for spenddown.
Return mail
04/01/2023
Terminations for whereabouts unknown
resume, effective no sooner than 04/30/2023.
See Returned Mail.
Change reporting
requirements and case actions
on reported changes
04/01/2023
Clients who report changes will have eligibility
redetermined, even if their renewal date
hasn’t approached.
Key takeaways
• Staff began requesting verification of income and other eligibility factors as of
04/01/2023, unless verified through electronic data sources.
• Change reporting requirements and case action on reported changes resumes.
• Some terminations occurred 04/30/2023, but more likely on or after 05/31/2023.
19
Notices for newly-eligible
Medicare clients
04/01/2023
Clients on Apple health for Adults who
become eligible for Medicare on or after April
2023 will be sent a notice to apply at DSHS.
Terminations resume for
Medicare-eligible clients
04/30/2023
Terminations of Apple Health for Adults for
being Medicare-eligible.
Post-eligibility reviews (PER)
HCA resumed its PER process in April 2023. Any changes to a client’s Apple Health eligibility occur
no sooner than 04/30/2023. HCA will use a redesigned PER notice developed with the Consumer
Notices Workgroup and the new envelope (see appendix 2).
ProviderOne extensions
Some clients lost coverage in Washington Healthplanfinder and could not be reinstated in that
system. Their coverage was extended in ProviderOne. These clients:
• Turned 19 and their immigration status does not qualify them for ongoing Apple Health,
or
• Received 12 months’ post-partum coverage and their immigration status does not qualify
them for ongoing Apple Health.
HCA will send a unique form to determine their continued eligibility when the PHE ends. See
appendix 5 for copy of the letter.
Redetermination occurs between May 2023 and April 2024. The due date for the form is the 5
th
of the following month. HCA will review the case file to determine if the client responded.
• No response received: Staff manually send a termination notice from Washington
Healthplanfinder with at least 10 days’ notice, and ProviderOne coverage ends at the end
of the month.
• Response received: Staff redetermine ongoing eligibility and send applicable eligibility
notices. This may include a termination notice from Washington Healthplanfinder with at
least 10 days’ notice, and ProviderOne coverage ends at the end of the month.

20
After-Pregnancy Coverage (APC)
Substitute Senate Bill (SSB) 5068 directed HCA to extend post-partum coverage to 12 months.
HCA implemented After-Pregnancy Coverage in July 2022. Clients within 12 months of the end of
their pregnancy end date will stay on Apple Health coverage until the end of their 12-month post-
partum period when they will go through the MAGI renewal process explained above.
It is important for a client to update their Healthplanfinder application to reflect their current
pregnancy status or the date their pregnancy ended.
Alien Emergency Medical (AEM) – MAGI
Once the PHE ends, AEM clients follow the MAGI renewal process above. AEM clients extended
three months at a time will have a renewal due between May 2023 and July 2023. Clients who do
not respond will terminate for not renewing.
Note: Coverage under AEM of COVID-19 testing and treatment ended May 11, 2023. Inpatient
hospital services relating to COVID-19 testing and treatment are still covered.
Foster care (FC) and adoption support (AS)
HCA’s Foster care and adoption support (FCAS) team maintain Apple Health for children in foster
care (FC), receiving adoption support (AS), and those under age 26 who age out of foster care.
During the PHE
Children in FC or AS who had a change in circumstances remained eligible for coverage even if FC
or AS ended. Children who age out of FC move to Former Foster Care Apple Health coverage until
they turn 26. Staff moved clients who turned 26 during the PHE to Apple Health for Adults.
Children in an institution, including in Children’s Long Term Inpatient Program (CLIP) facility or
hospital, for 30+ days, remained on their program.
21
Unwinding
Clients who moved to MAGI Apple Health for Adults or Apple Health for Kids in Washington
Healthplanfinder will have their eligibility redetermined based on their renewal end date or
change report. See the Renewals – MAGI section above.
Clients released from an institution more than 12 months ago will have their eligibility
redetermined by HCA FCAS staff. FCAS staff can be reached Monday through Friday from 7:30
a.m. to 5 p.m. at 1-800-562-3022, extension 15480 or email [email protected].gov.
Moving to a Qualified Health Plan
If a client is no longer eligible for Apple Health, Washington Healthplanfinder offers coverage of
Qualified Health Plans with financial help to lower their premiums. Individuals and families who
lose Apple Health can sign up for a health plan through wahealthplanfinder.org, in the 60 days
before or after their Apple Health coverage end date. New coverage for clients who sign up
during this special enrollment period will begin the day after their Apple Health coverage end
date unless a later start date is requested.
Clients who are unable to enroll within 60 days of their Apple Health coverage end date have
additional opportunities to get covered. Those earning up to 250% of the federal poverty level
(up to $34,000 annually for an individual and $70,000 for a family of four) may qualify for the
Cascade Care Savings special enrollment period. This allows Washingtonians to enroll in a high-
quality Cascade Care plan for less than $10 a month by using Cascade Care Savings, Washington’s
new state-funded premium financial assistance. These plans, offered by all Washington
Healthplanfinder insurance companies, have lower deductibles, and cover important services like
primary care visits, mental health services, and generic medications with low co-pays before the
deductible.
Clients may also qualify for special enrollment periods based on qualifying life events including
job loss, income changes, and household changes (birth, adoption, marriage, and more). Clients
who lose Apple Health coverage during the Medicaid unwind who are unable to use an existing
special enrollment period can request that their circumstances be reviewed, which Washington
Healthplanfinder will do on a case-by-case basis.

22
For help enrolling in coverage, clients should call the Washington Healthplanfinder Customer
Support Center at 1-855-923-4633 (TTY 1-855-627-9604) or find help in their community from
Washington Healthplanfinder enrollment partners. Free language assistance is available in over
200 languages.
Note: If Apple Health coverage terminates for not responding or not completing a renewal clients
will not be able to take advantage of the ARP savings until they reapply and are eligible.
23
Chapter 3: Moving between Classic and
MAGI Apple Health programs
Apple Health for Adults (N05) and 65+ or Medicare-eligible
During the PHE
Clients on MAGI Apple Health for Adults who turned age 65 or became Medicare-eligible received
notice to apply for ongoing Apple Health at DSHS. If they responded, N05 ended, but staff opened
SSI-related medical with DSHS. If they did not respond, the system extended eligibility 3 months
at a time.
Unwinding
Clients extended on MAGI Apple Health for Adults who are age 65 or older or Medicare-eligible
will be included in the May, June, and July MAGI renewals. HCA will mail these clients an
additional notice (appendix 6). If they do not respond by applying through DSHS, the
redetermination process is complete and Apple Health coverage ends. Clients will receive notice
that their Apple Health coverage closed, and they can apply at DSHS anytime. HCA will also stop
covering Medicare premiums when Apple Health ends, unless the client qualifies for a Medicare
Savings Program.
SSI terminations
Clients who receive Supplemental Security Income (SSI) automatically receive SSI medical through
DSHS.
During the PHE
If a client’s SSI ended, DSHS continued clients on SSI medical.
Unwinding
DSHS will resume the SSI redetermination processes by sending clients updated notices to apply
at Washington Healthplanfinder or Washington Connection for continued coverage. If the client
does not act, SSI medical ends.
24
MAGI Apple Health and LTSS
Some clients extended on MAGI Apple Health programs receive long-term services and supports
(LTSS) administered by HCS and DDA. HCA provides HCS monthly reporting for MAGI closures for
clients accessing LTSS. Public benefit specialists and social service case management staff at HCS
will assist clients with applications and necessary verifications as they are redetermined for Apple
Health through DSHS. Assigned HCS and DDA staff follow equal access policy and contact clients if
their annual eligibility review is not received.
25
Chapter 4: Other Classic and MAGI Apple
Health program information
The following sections apply to both Classic and MAGI Apple Health clients.
Language access
HCA, DSHS, and Washington Healthplanfinder provide written and verbal translation and
interpreter services free of charge, including to clients who are deaf or hard of hearing.
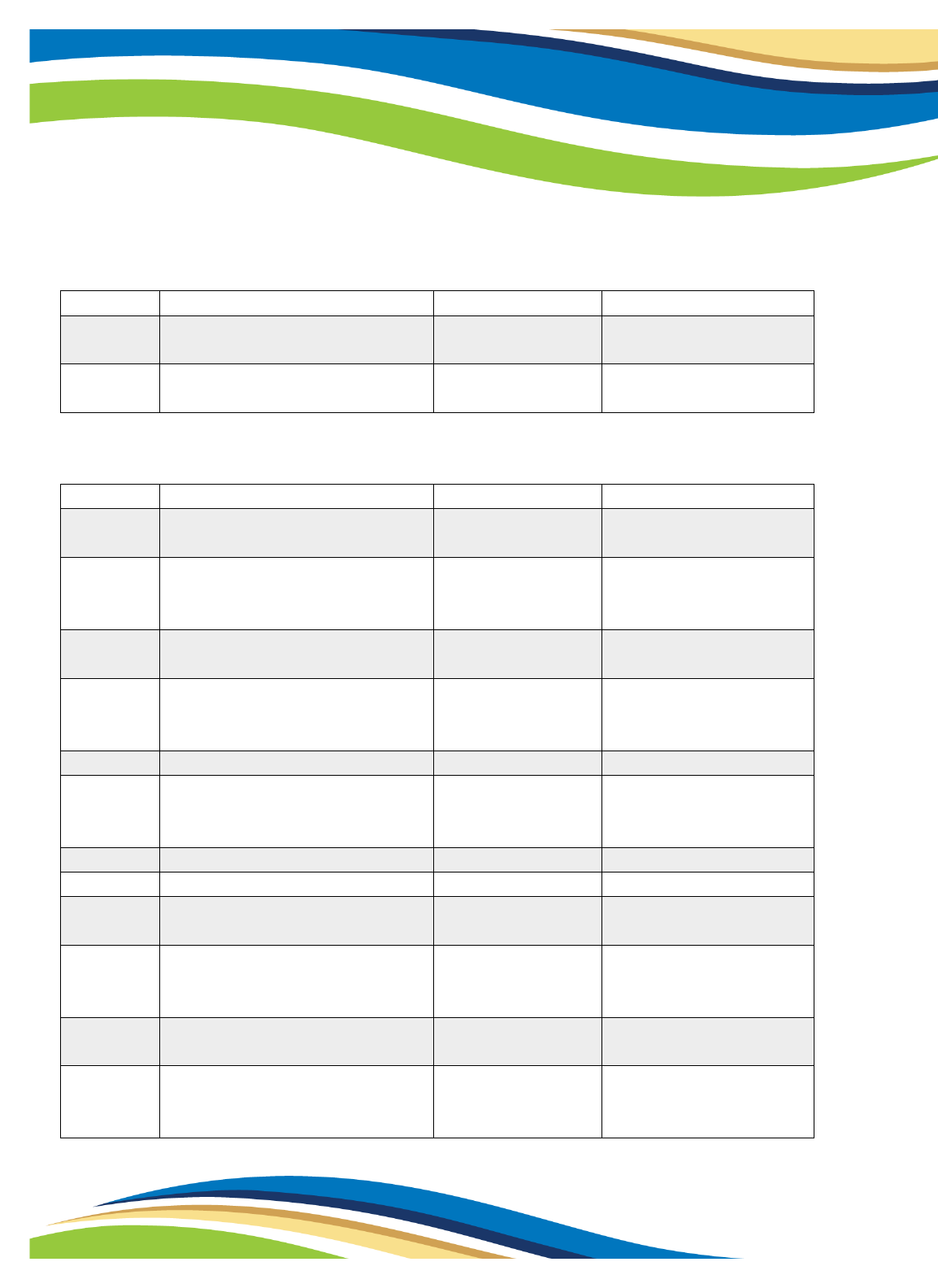
CHIP and HWD premiums
Procedure
Date
Details
CHIP postcard for premiums
resuming
05/15/2023
CHIP clients receive a postcard advising them
of premium collection resuming and which
monthly invoice to pay.
HWD postcard for premiums
resuming
06/01/2023
HWD clients receive a postcard advising them
of premium collection resuming and which
monthly invoice to pay.
Premium requirements
resume
07/2023
HCA will update invoice language to explain
premium requirements resuming.
CHIP terminations for non-
payment of premium
09/30/2023
First round of post-PHE terminations for not
paying premium
Key takeaways
• Apple Health for Workers with Disabilities (HWD) and Apple Health for kids with
premiums (also known as the Children’s Health Insurance Program or CHIP) premium
requirements resume July 2023.
• Clients who are American Indian/Alaskan Native do not have to pay a premium.
26
HWD terminations for non-
payment of premium
12/31/2023
First round of post-PHE terminations for not
paying premium
Public charge
Clients can receive Apple Health coverage and emergency medical care without impacting their
ability to become a Lawful Permanent Resident in the future.
Currently, the only health benefit that immigration officials can consider for the public charge
test is government-funded long-term institutional care, such as care received in a nursing facility.
Alien Emergency Medical (AEM) and state-funded programs are excluded from reporting under
public charge.
HCA will continue to protect the confidentiality of each client’s personal information and does
not share this information unless required by law.
Appeals
Clients who disagree with a decision by HCA or DSHS to terminate, change, or deny Apple Health
coverage have the right to appeal. This is called an administrative hearing, which is a legal process
where a judge reviews an agency decision. Clients may be able to keep their Apple Health
coverage during the appeal process, if they request an appeal within 10 days from the date of the
notice or by the end of the month of the notice, whichever is later.
Find out more information on Apple Health appeals.
Reconsideration
Clients who received a termination notice have until the end of that month of the notice to
submit all information to have their eligibility reconsidered. Clients may reapply for coverage at
any time.
Returned renewal mail
If the United States Postal Service (USPS) returns a renewal or eligibility review notice as
undeliverable, HCA and DSHS staff will attempt to contact the household to obtain a valid

27
address. Staff will attempt to contact the household through two methods when available,
including by phone or email. Clients may be given additional time to complete their renewal if
USPS returns the original renewal or eligibility review notice.
When USPS returns mail with an in-state forwarding address, staff update all systems with the
new address and remail the returned notices to the new address. If the forwarding address is out-
of-state, staff send a letter requesting verification of residency.
Upcoming webinars
HCA hosted several webinars to review unwinding activities. Find our previous webinars on our
Webinars, video, and presentations page. Sign up for GovDelivery to register for webinars and
receive weekly updates.
Contact
Email AHEligCovid19@hca.wa.gov if you’d like to arrange a time for review or address any
questions, comments or concerns. View the Cross Agency Desk Aid for more information.
Clients with questions should contact the agency that determined their eligibility:
• Washington Healthplanfinder Customer Support Center
Monday to Friday 7:30 a.m. – 5:30 p.m.
Phone: 1-855-923-4633
TTY: 1-855-627-9604
Language assistance is available in more than 200 languages and disability
accommodations are provided at no cost.
Navigator search
• Apple Health through Washington Healthplanfinder:
HCA Medical Eligibility Determination Services (MEDS)
Email MEDS
Contact Us
Phone: 1-800-562-3022
Monday to Friday 7 a.m. – 5 p.m., except state holidays
28
HCA community-based specialists for assistance in your area
• Foster care, adoption support, and alumni Apple Health through Foster Care and Adoption
Support (FCAS) staff:
Email FCAS
Phone: 1-800-562-3022, extension 15480
Monday to Friday 7:30 a.m. – 5 p.m., except state holidays
• Classic Apple Health (non-MAGI) through DSHS – CSD:
Phone: 1-877-501-2233
Monday to Friday 8 a.m. – 3 p.m., except state holidays
• Classic Apple Health (non-MAGI) through DDA (cases in office 017):
Phone: 1-855-873-0642
Monday to Friday 8:00 a.m. – 5 p.m., except state holidays
• Classic Apple Health and Long Term Service and Supports (non-MAGI) through HCS:
Contact Local HCS office (may take a minute to load)
Outreach
HCA’s outreach plan includes:
1) A postcard mailed the month before renewal and eligibility reviews are sent. The postcard
is to encourage the client to update their address and phone number.
2) Updated language to renewal and eligibility review notices explaining the need to respond
now that the PHE-related extensions are ending.
3) Text messages to clients at-risk of termination for not completing a renewal or eligibility
review. See hca.wa.gov/ah-texts for more information.
4) Automated phone call to clients at-risk of termination for not completing a renewal or
eligibility review.
5) Member outreach from managed care plans.
More information on outreach can be found in HCA’s End of PHE Communications Toolkit.
29
Apple Health ambassador program
HCA’s new Apple Health ambassador program uses community organizations and influencers to
act as volunteer Apple Health ambassadors! Ambassadors will work to ensure that Apple Health
clients have the information and resources needed to maintain coverage at the end of the
continuous coverage requirement period.
More information can be found on our Apple Health ambassador page.
MCOs and 834 information
HCA worked with managed care organizations (MCOs) to conduct member outreach to ensure
clients respond to renewal notices. The 834 file is a standard report sent from HCA to the MCOs
containing the MCO’s member information.
When a client is auto-renewed, the next daily 834 file will show a new recertification end date.
The auto-renewal process ends on or before the 10th of every month so MCOs should begin
outreach to clients after the 11
th
. Additionally, as clients complete their renewal, the new
recertification end date will show in the next 834 file so renewal outreach does not need to be
conducted by the MCO.
For example, clients with a recertification end date of 11/30/2023 go through auto-renewal
October 1-10
th
. MCOs should use the 834 issued October 11
th
to see who is still due to renew
11/30/2023 and conduct outreach. When a client manually renews, their new recertification end
date will appear on the next daily 834 file.
Another enhancement for the 834 file is improved communication between HCA and the MCOs
on why clients are losing Apple Health eligibility. Depending on the reason for termination, MCOs
can conduct outreach to clients to reconnect them to Apple Health or other health insurance
options.
30
Appendices
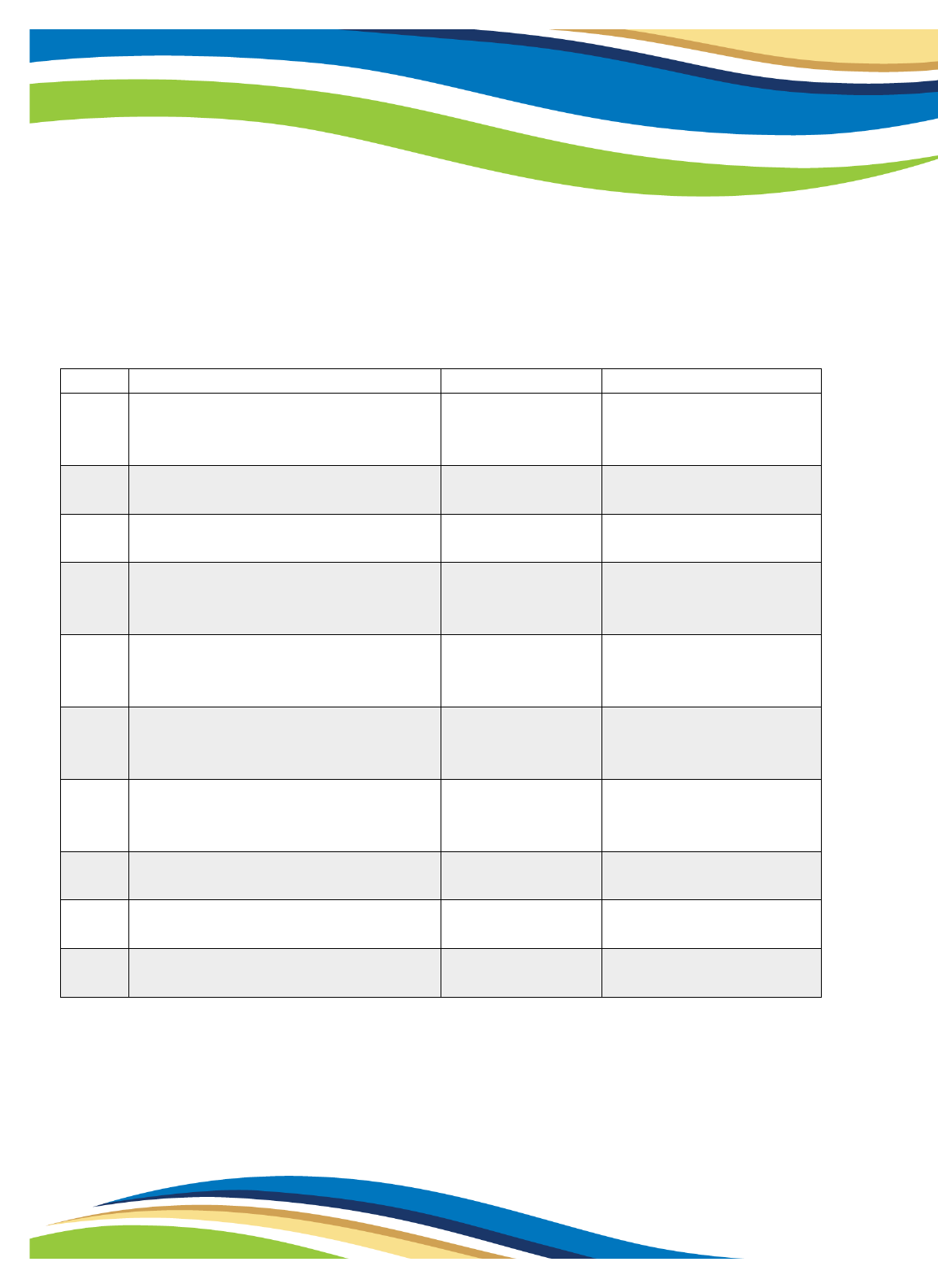
Appendix 1: Coverage groups
SSI and SSI-related Classic Apple Health, also called Aged/Blind/Disabled (ABD)
Group
Description
RAC(s)
Administering Agency
G03
Categorically Needy Non-
Institutional Medical in an Alternate
Living Facility
1046, 1047
DDA, HCS
S01
SSI recipients
1104, 1105, 1106,
1107
CSD
DDA, if client is in ARTF
S02
ABD Categorically Needy
1108, 1109, 1110,
1111
CSD
DDA, if client is in ARTF
S03
QMB Medicare Savings Program
(MSP) Medicare premium and co-
pays
1112, 1113
CSD if not receiving
services from HCS or
DDA
S04
QDWI Medicare Savings Program
1114
CSD if not receiving
services from HCS or
DDA
S05
SLMB Medicare Savings Program -
Medicare premium only
1115, 1116
CSD if not receiving
services from HCS or
DDA
S06
QI-1 Medicare Savings Program
1117, 1118
CSD if not receiving
services from HCS or
DDA
S07
Emergency Related Service Only
(AEM)
1119, 1120
CSD
S95
Medically Needy no spenddown
1124, 1125, 1126,
1127
CSD
S99
Medically Needy with spenddown
1124, 1125, 1126,
1127
CSD
31
SSI-related Healthcare for Workers with Disability
Group
Description
RAC(s)
Administering Agency
S08
Apple Health for Workers with
Disabilities CNP premium based
program
1121, 1134, 1271
DDA or HCS
Institutional Home and Community Based Waivers, and Hospice SSI and SSI-related
Group
Description
RAC(s)
Administering Agency
L21
DDD/HCS Waiver on SSI
1146, 1147, 1152,
1153, 1218, 1219,
1220, 1221
HCS or DDA
L22
DDD/HCS Waiver – gross income
under the SIL
1148, 1149, 1150,
1151, 1174, 1175,
1222, 1223, 1224,
1225
HCS or DDA
L24
Undocumented alien/non-citizen LTC
– residential placement.
1190, 1191, 1192,
1193, 1194, 1195
HCS
L31
PACE or hospice on SSI
1226, 1227, 1228,
1229, 1236, 1237,
1138, 1239
HCS if PACE DDA if
Hospice
L32
PACE or hospice – SSI-related
1230, 1231, 1232,
1233, 1234, 1235,
1240, 1241, 1242,
1243
HCS if PACE DDA if
Hospice
L41
Roads to Community Living on SSI
1260, 1261, 1262,
1263
HCS or DDA
L42
Roads to Community Living – SSI
related
1264, 1265, 1266,
1267, 1268, 1269
HCS or DDA
Non-Institutional Community First Choice – Personal care services in the community
Group
Description
RAC(s)
Administering Agency
L51
Community First Choice (CFC) on SSI
1104, 1105, 1106,
1107, 1244, 1245,
1246, 1247
HCS or DDA
32
Group
Description
RAC(s)
Administering Agency
L52
Community First Choice (CFC) – SSI
related at home or in an ALF
1046, 1047, 1108,
1109, 1110, 1111,
1248, 1249, 1250,
1251, 1252, 1253,
1254, 1255, 1256,
1257, 1258, 1259
HCS or DDA
SSI-related: Residing in a medical institution 30 days or more
Group
Description
RAC(s)
Administering Agency
L01
SSI recipient in a medical
institution - residing in a
medical institution 30 days or
more
1065, 1066, 1067,
1068, 1069, 1070,
1168, 1169
HCS or DDA
L02
SSI related CNP in a medical
institution income under the
SIL
1071, 1072, 1073,
1074, 1162, 1163,
1164, 1165
HCS or DDA
L04
Undocumented alien/non-
citizen LTC must be pre-
approved by ADSA program
manager. Emergency Related
Service Only (45 slots)
1077, 1078, 1081,
1082, 1158, 1159,
1160, 1161, 1182,
1183, 1184, 1185
HCS
L95
SSI related Medically Needy
no spenddown. Income over
the SIL. Income under the
state rate.
1083, 1084, 1085,
1086, 1087, 1186,
1187, 1154, 1155,
1156, 1157, 1166
HCS or DDA
L99
SSI related Medically Needy
with spenddown
Income over the SIL. Income
over the state rate but under
the private rate. Locks into
state NF rate.
1083, 1084, 1085,
1086, 1087, 1088,
1089, 1090, 1091,
1092, 1154, 1155,
1156, 1157, 1167,
1186, 1187, 1188,
1189,
HCS or DDA
33
Institutional Family/Children
Group
Description
RAC(s)
Administering Agency
K01
Categorically Needy family in
medical institution
1052, 1053, 1054,
1055
MEDS
K03
Undocumented alien family in
medical institution
Emergency Related Service Only
1056, 1176, 1057,
1177
MEDS
K95
Family LTC Medically Needy no
spenddown in medical
institution
1059, 1060, 1179,
1061, 1062, 1180
MEDS
K99
Family LTC Medically Needy
with spenddown. In medical
institution
1059, 1060, 1179,
1061, 1062, 1180
MEDS
Family Planning
Group
Description
RAC(s)
Administering Agency
P05
P06
Family Planning
1097, 1098, 1099,
1100, 1101, 1272
MEDS
Refugee Coverage
Group
Description
RAC(s)
Administering Agency
R02
Transitional 4-month extension
1103
CSD
R03
Refugee Categorically Needy
1103
CSD
Foster Care and Adoption Support
Group
Description
RAC(s)
Administering Agency
D01
SSI recipient FC/AS/JRA
Categorically Needy
1014, 1015, 1016,
1017, 1018
MEDS
D02
FC/AS/JRA Categorically Needy
1019, 1020, 1021,
1022, 1023
MEDS
D26
Title IV-E federal foster care
1196
MEDS
34
Family/Children spenddown
Group
Description
RAC(s)
Administering Agency
F99
Medically Needy children
spenddown
1039, 1040
MEDS
P99
Medically Needy pregnant
spenddown
1101, 1102
MEDS
MAGI Apple Health
Group
Description
RAC(s)
Administering Agency
N01
Apple Health for
Family/Caretaker Relatives
1197
MEDS
N02
Apple Health for
Family/Caretaker Relatives –
12-month Extension
1198
MEDS
N03
Apple Health for Pregnant
Clients
1199, 1200
MEDS
N04
Apple Health After-Pregnancy
Coverage (on Apple Health
when pregnancy ended)
1274, 1275
MEDS
N05
Apple Health for Adults
1201, 1217
MEDS
N07
Apple Health After-Pregnancy
Coverage (applied after
pregnancy ended)
1276
MEDS
N10
Apple Health for Newborns
1202
MEDS
N11
Apple Health for Kids
1203, 1204, 1205
MEDS
N13
Apple Health for Kids with
Premiums (CHIP)
1206, 1207
MEDS
N21
Apple Health for
Family/Caretaker Relatives,
AEM
1208
MEDS
N23
Apple Health for Pregnant
Clients, non-citizens
1209
MEDS
N24
Apple Health After-Pregnancy
Coverage non-citizens (on Apple
Health when pregnancy ended)
1277
MEDS
35
Group
Description
RAC(s)
Administering Agency
N25
Apple Health for Adults, AEM
1210
MEDS
N27
Apple Health After-Pregnancy
Coverage non-citizens (applied
after pregnancy ended)
1278
MEDS
N31
Apple Health for Kids, non-
citizens
1211
MEDS
N33
Apple Health for Kids with
Premiums (CHIP), non-citizens
1212, 1213
MEDS
Medical Care Services
Group
Description
RAC(s)
Administering Agency
A01
MCS Medical Care Services –
non-citizen
(Aged/Blind/Disabled)
1214, 1215
DSHS
A05
MCS Medical Care Services –
non-citizen (under 65,
incapacitated)
1216
DSHS
A24
MCS for Survivors of Certain
Crimes
1216
DSHS
Breast and Cervical Cancer Program
Group
Description
RAC(s)
Administering Agency
S30
Breast and Cervical Cancer
Program (BCCTP)
1122, 1123
MEDS
Tailored Supports for Older Adults
Group
Description
RAC(s)
Administering Agency
T02
TSOA – no medical benefits
issued
3199
HCS
36
Appendix 2: MAGI renewal notices, PER notice, and outreach
New enhanced envelope
Effective April 2023, when Washington Healthplanfinder mails these two letters to a client
receiving mail via USPS, it will use the following envelope:
• Response Required: Apple Health Request for Information (EE005)
• Response Required: Apple Health Renewal (EE009)
37
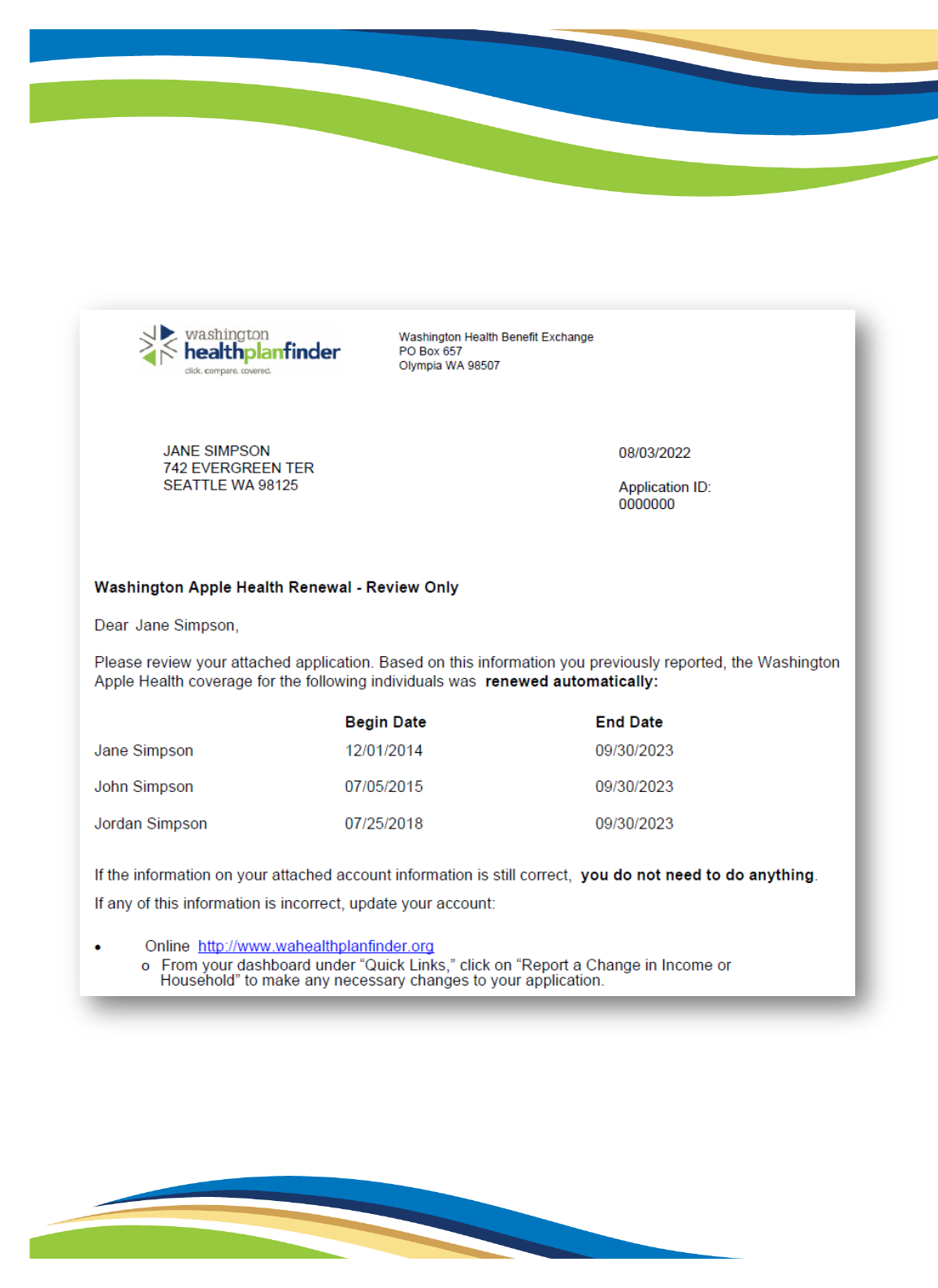
Washington Apple Health Renewal – Review Only (EE008)
Clients successfully auto-renewed receive this notice:
38
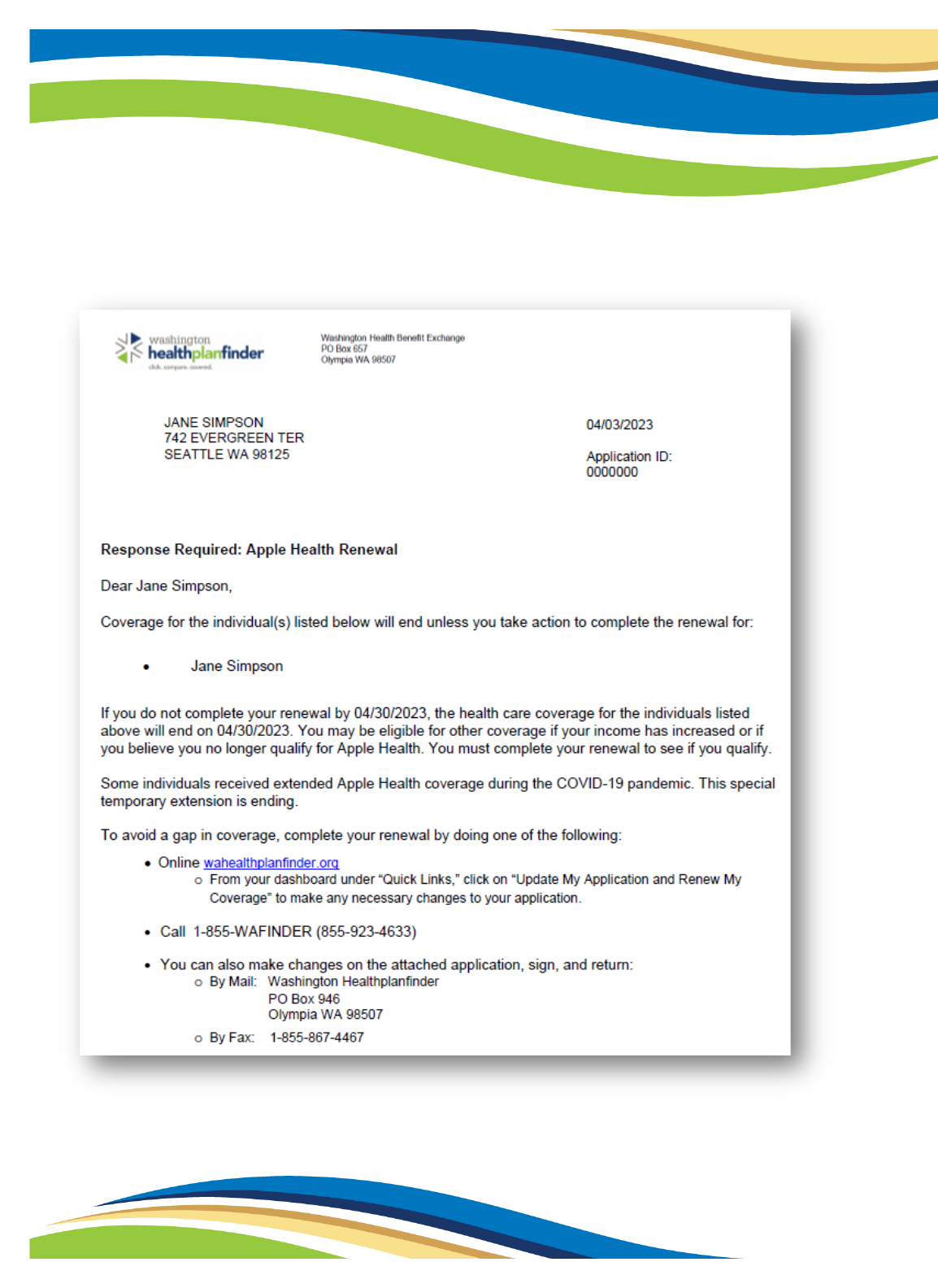
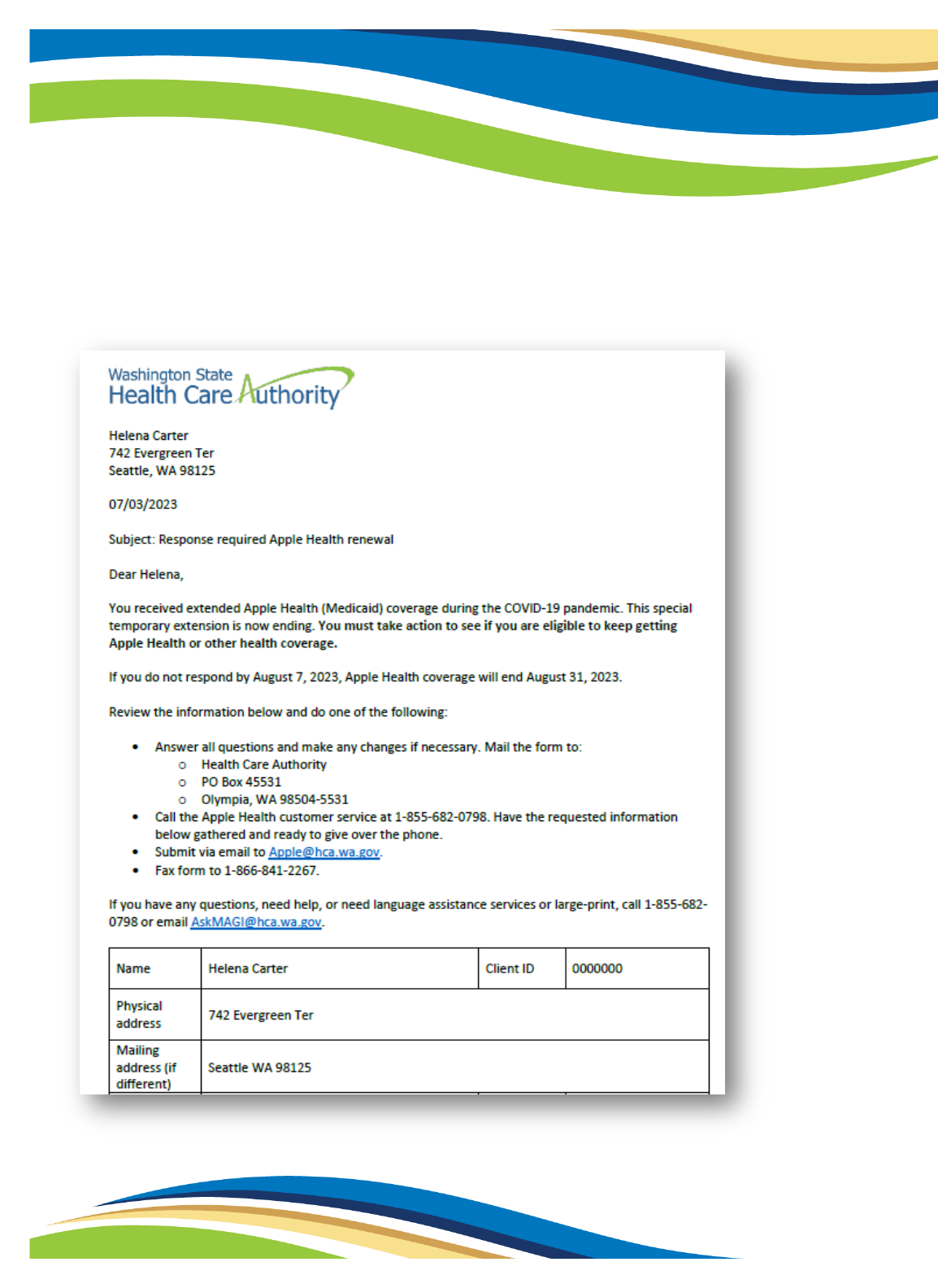
Response Required: Apple Health Renewal (EE009)
Clients who could not be auto-renewed and must take action receive this notice:
39
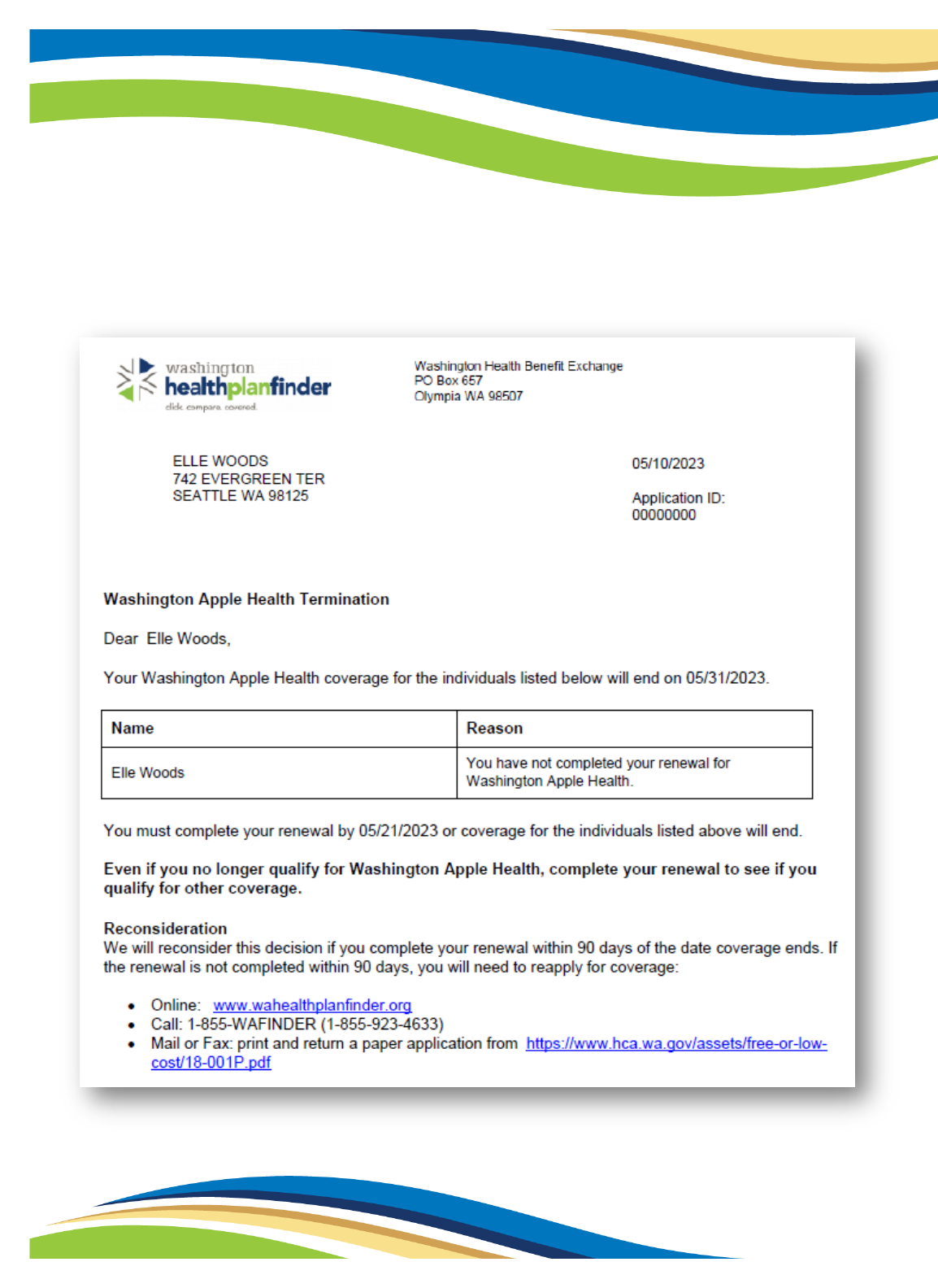
Washington Apple Health Termination (EE011)
Clients whose Apple Health is ending. In this example, the client did not complete their
renewal.
40
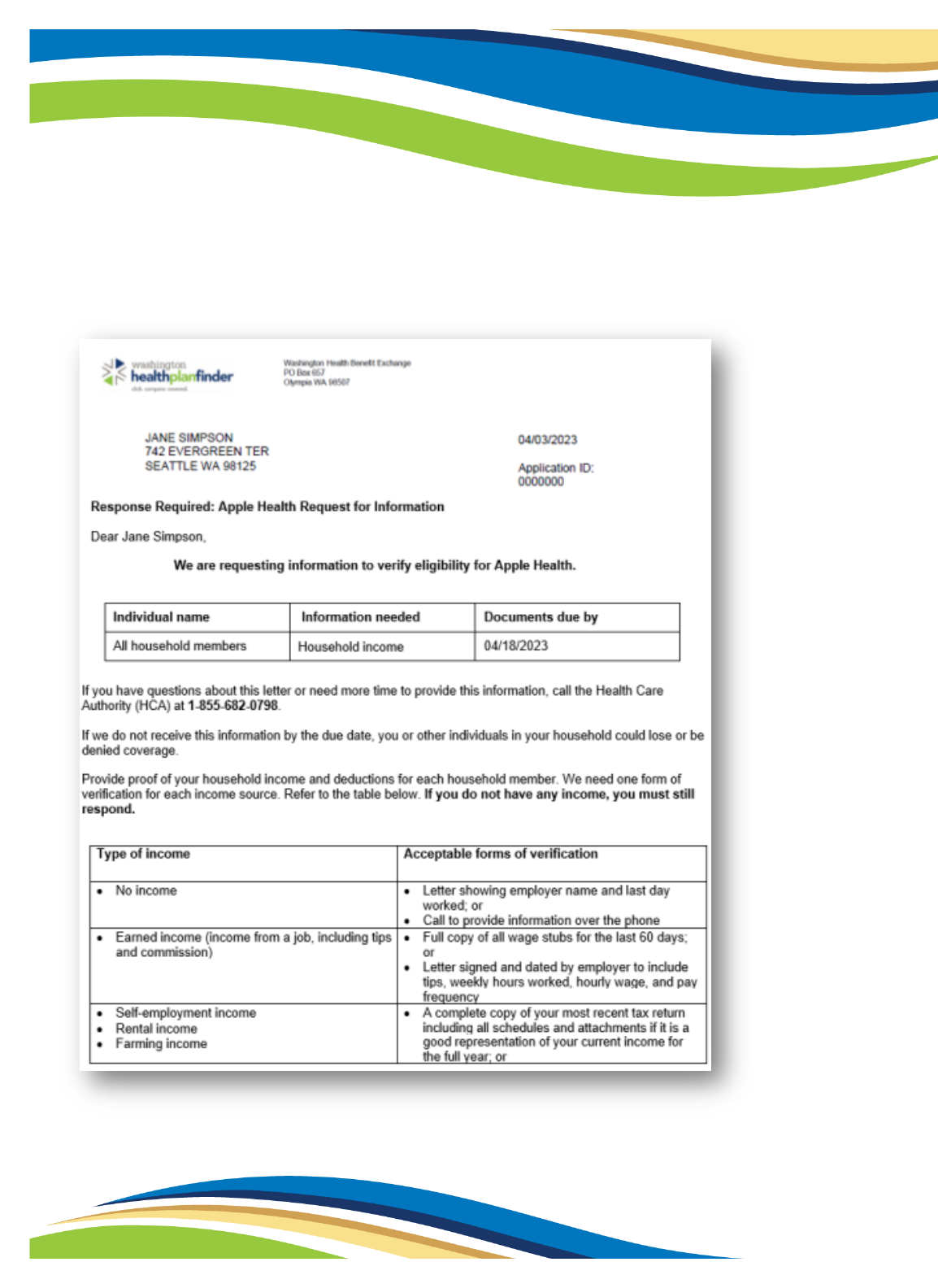
Post-Eligibility Review – Response Required: Apple Health Request for Information (EE005)
Clients who apply or renew may need to respond to this PER notice:

41

42
Response Required: Apple Health Request for Information (EE005)
Clients who apply or renew may need to provide other verification
43
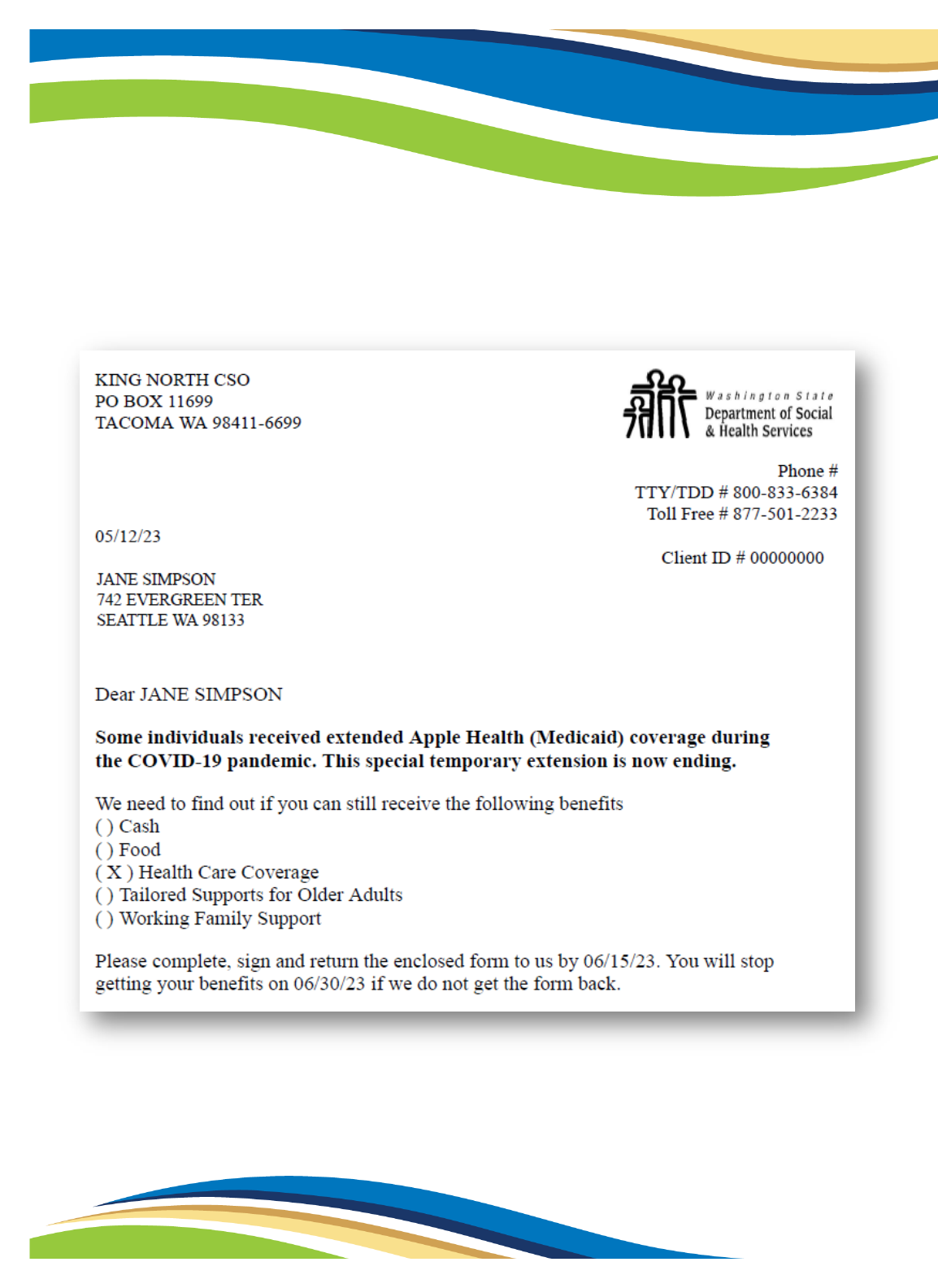
Appendix 3: Classic Eligibility Review notices and outreach
Mail-in Eligibility Review (0022-01)
The ER is mailed to clients receiving services from DSHS – CSD:
44
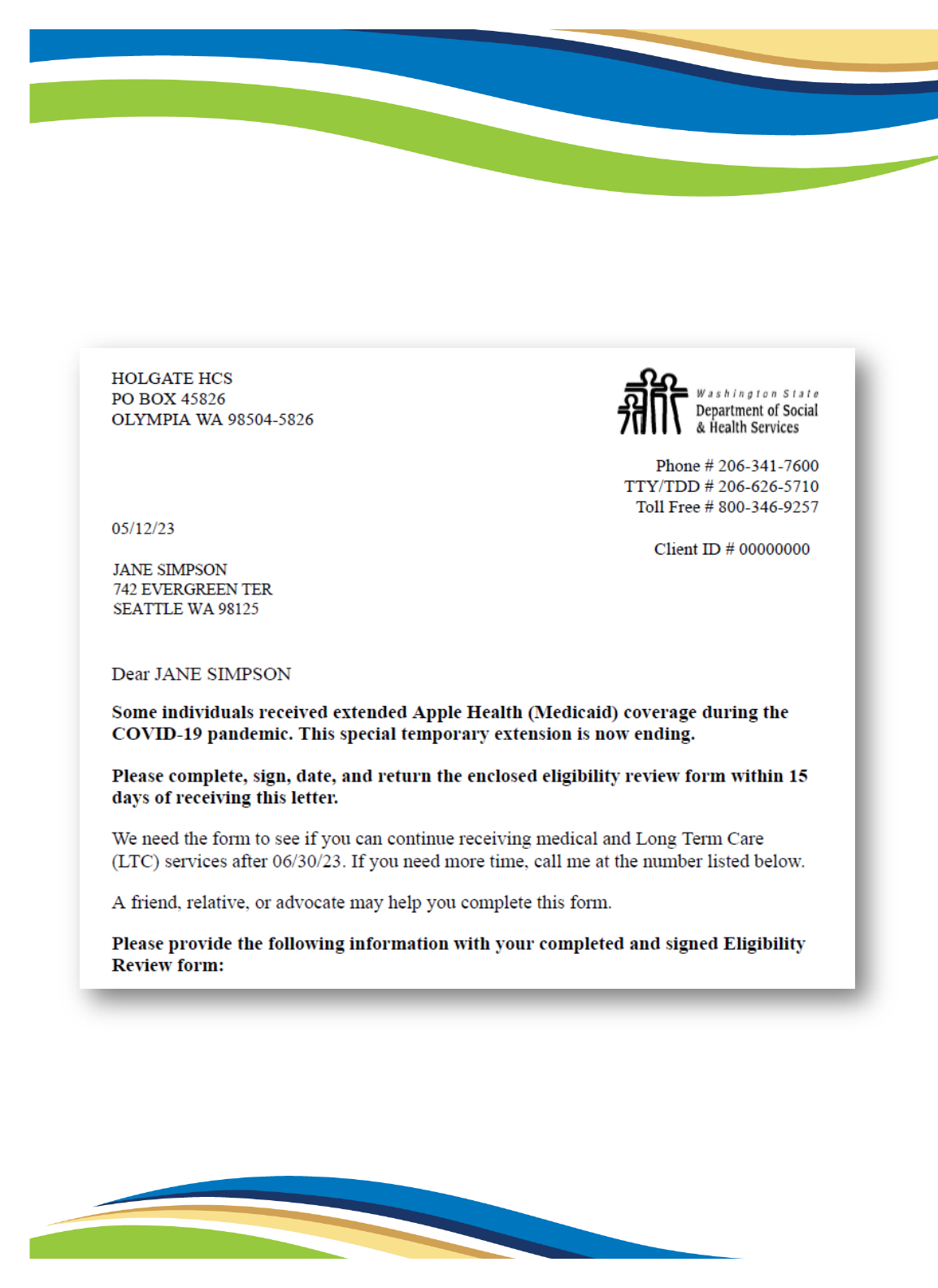
Mail-in Eligibility Review (0022-04)
The ER is mailed to clients receiving services from DSHS – HCS or DDA:
47
Appendix 5: Redetermination Notice to ProviderOne extensions
ProviderOne redetermination notice
Notice sent to clients extended in ProviderOne only
48
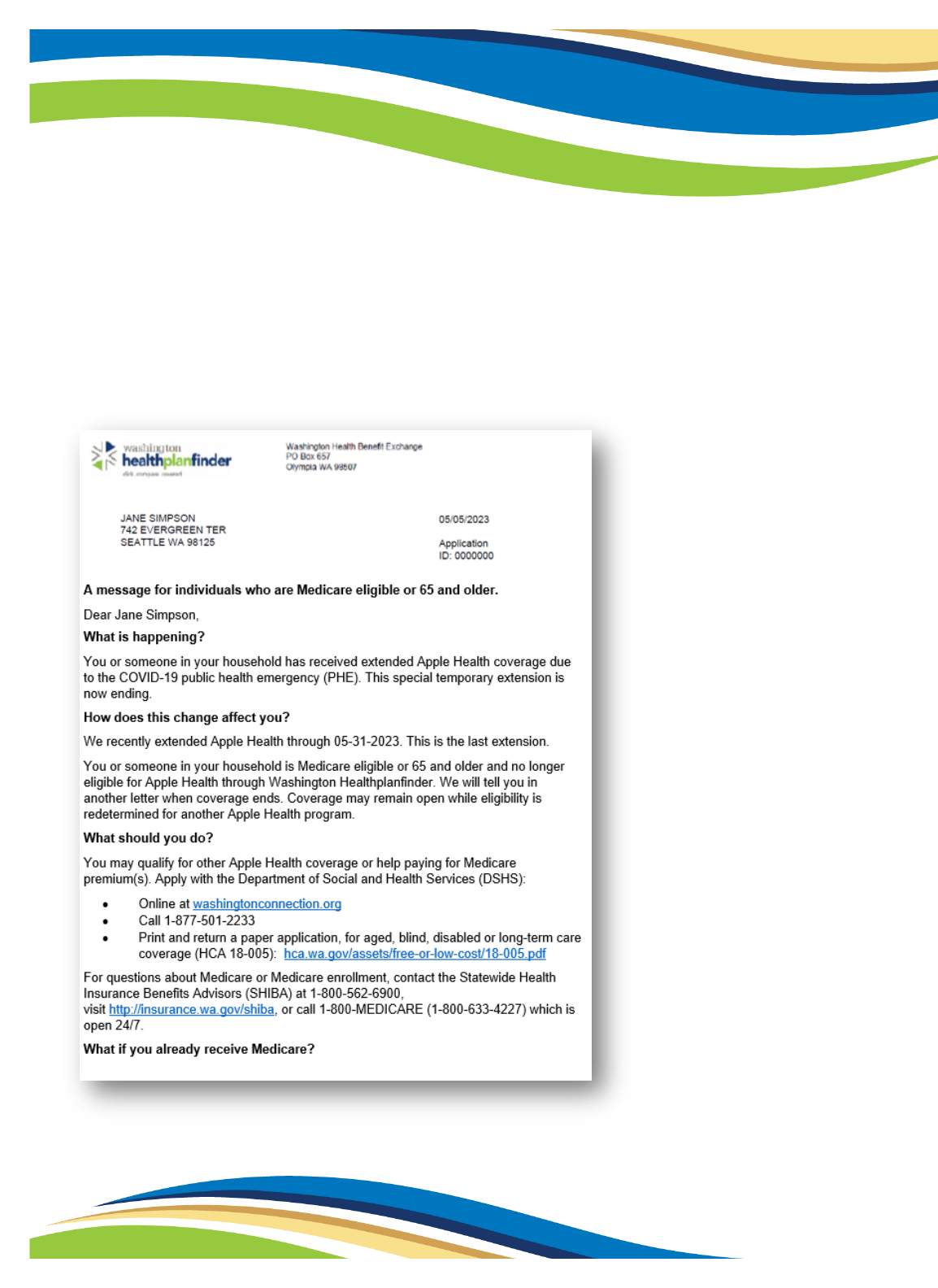
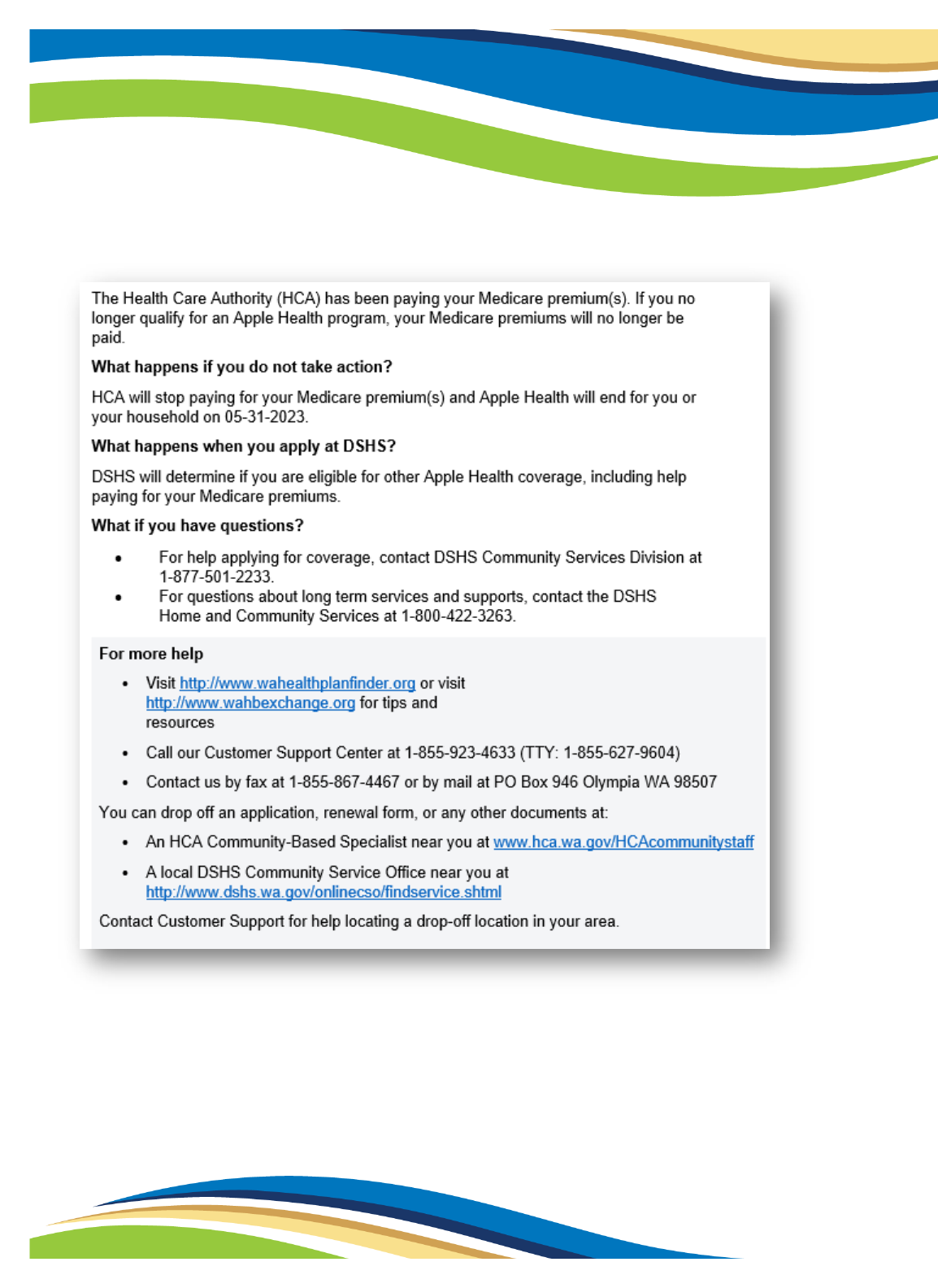
Appendix 6: Notice to MAGI Apple Health for Adults who are 65+
or Medicare eligible
Medicare FAQ notice
Notice sent to clients active on Apple Health for Adults who are Medicare eligible or 65+
49

52
Appendix 8: Acronyms
AEM Alien Emergency Medical
ALTSA Aging and Long-Term Support Administration, part of DSHS
APC After-Pregnancy Coverage
ARPA American Rescue Plan Act
ARTF Adult Residential Treatment Facility
AS Adoption support
CHIP Children’s Health Insurance Program (Apple Health for Kids with Premiums)
CLIP Children’s Long-Term Inpatient Program
CMS Centers for Medicare & Medicaid Services
COFA Compact of Free Association
CSD Community Services Division, part of DSHS
DDA Developmental Disabilities Administration, part of DSHS
DSHS Department of Social and Health Services
ER Eligibility review
FC Foster care
FCAS Foster care and adoption support
FFCRA Families First Coronavirus Response Act
HBE Washington Health Benefit Exchange
HCA Health Care Authority
HCS Home and Community Services, part of DSHS
HHS United States Department of Health and Human Services
HWD Apple Health for Workers with Disabilities
LTSS Long-term services and supports
MAGI Modified Adjusted Gross Income

53
MACSC Medical Assistance Customer Service Center, part of HCA
MCO Managed care organization
MEDS Medical Eligibility Determination Services, part of HCA
OE Open enrollment
OIC Office of the Insurance Commissioner
OMEP Office of Medicaid Eligibility and Policy, part of HCA
PER Post-eligibility review
PHE Public health emergency
QHP Qualified health plan
SEP Special enrollment period
SHIBA Statewide Health Insurance Benefits Advisors, part of OIC
SSI Supplemental Security Income, differs from SSDI
WAC Washington Administrative Code